Physical Therapy EMR Automation Tools | Making Documentation Easier
That documentation is not a popular task for anyone including for physical therapists is well known. But if the documentation helps improve outcomes and if EMR automation tools make it faster and easier to perform documentation then therapists are more likely to come on board. Clinical documentation should be as painless and easy to complete as possible. The physical therapy EMR should play a significant role here.
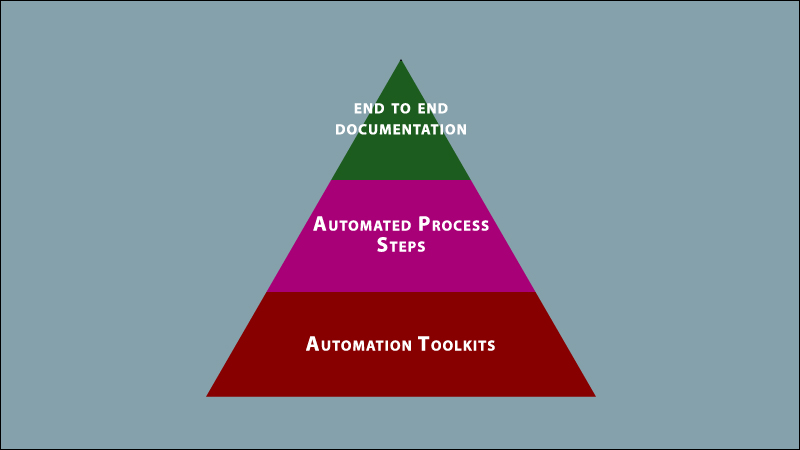
Automation Toolkit
Automation has several flavors. The following basic tools should be table stakes for any physical therapy EMR.
Clinical Templates
Productivity boosters would include a clinical library of templates that could be tailored anytime with distinct types of questions. These templates could be saved as personal templates or as company level templates.
Short Codes
Short codes that auto populate text are another automation feature to update the note rapidly and automatically.
Copying Forward Notes
Automatically carrying forward text from a previous note that could subsequently be changed or modified as needed is another automation example.
Notes Compliance Checks
If required questions are not filled out, then the EMR should prevent the clinician from locking and signing off on the note. This would ensure compliance with clinic and regulatory standards.
Patient Information Card
A patient information card that lists potential showstoppers like missing/expiring authorizations would help focus on the things that matter.
Scoring Tables
Scoring tables for standardized outcome tests built into the system would ensure that outcome measures are effectively tracked.
Document Faxing
Automatically faxing notes to the referring provider/payer on file by seamlessly merging data from the patient record would be another task to not have to worry about. Weaving these automation tools into the end-to-end documentation sequence should make the process faster and more efficient.
Automated Process Steps
Firstly, automation tools should be used to build key documentation steps.
Outcomes Reporting
When it comes to outcomes tools, there are patient reported outcomes and outcomes that are updated by the therapist in consultation with the patient. Patient reported outcomes questionnaires could be sent to patients ahead of their visit as part of their intake paperwork, right from the EMR. This could include, for example, shoulder pain and disability index for shoulder injury. Outcomes would be updated by directly entering scores based on which the EMR would automatically calculate impairment. Alternatively, the therapist could go through the examination together with the patient or the outcomes survey could be handed to the patient on a tablet when in the clinic.
Goals And Other Tests
Range of motion and other special tests could also be part of the note. Range of motion values could be pre-saved on the template as normative values. Adding personalized goals from a goal bank with tracking goals would make progress tracking easier: goals met, goals mastered, and goals in progress. Goals would be set on the initial evaluation and reviewed on every visit.
Putting Automation to Work
Finally, the process steps and tools would come together to help therapists to complete end-to-end documentation sequences.
Initial Evaluation
After the therapist completes the initial evaluation, it could be automatically converted into a streamlined, one page plan of care. Another automation example would be an automated progress note that copies forward the previous progress report or evaluation.
Daily Note
A key part of documentation would be the daily note. This is a combination of the exercise flowsheet (times, sets, reps), daily SOAP note itself, and charges. Exercise programs could be preloaded in the flowsheet with the option to roll forward values from earlier sessions. This would automatically check off exercises done on previous visits with times and number of sets and reps that could then be modified or reordered. It would also be possible to see history data for an individual exercise that shows how the patient has progressed over time. The daily SOAP note could be rolled forward from the previous encounter and updated. All sections of the SOAP note could be copied forward. The combined document then becomes the updated daily note.
Charges Entry
Charges would get automatically baked into the template with codes that match up with evals and disciplines, ICD pointers would get attached, and place of service codes would be driven by the appointment. Payer specified modifiers and place of service code rules would automatically set the right modifiers and settings.
Discharge Note
The discharge note would be copied forward from the progress note. The previous progress note would be updated for the discharge encounter after adding the date of discharge and who the patient is discharged by, therapist, referring doctor, or insurance. Automation at each stage kicks in to ensure that speed and efficiency are optimized and that therapists get to focus on what matters most, which is of course patient care.